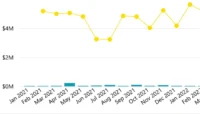
CrossFit Athlete Demographic Distribution Report
CrossFit is a dynamic and fast-growing industry where data can play a powerful role in driving business performance. While CrossFit gyms aren’t currently clients of LeapFrogBI, we created this report using sample data as a project to explore how analytics could support gym owners in making smarter decisions.